Generically, the clinical syndromes that result from alterations in hemoglobin (Hb) are known as hemoglobinopathies and several laboratory tests are interpreted to know them, of which the most relevant is Hb electrophoresis (EF).
The human Hb 1 molecule is formed by 2 pairs of globin chains, and a heme molecule is attached to each of them. Physiologically, 6 variants are formed: Three transient embryonic variants, called Hb Gower 1, Hb Gower 2 and Hb Portland, HbF, which is the predominant in fetal life, HbA, which constitutes more than 95% of adult Hb and HbA2, also present in a lower percentage (1-3.5%) in children and adults.
There are many Hb variants genetically determined (inherited) and although most are harmless, others cause remarkable clinical alterations.
The hemoglobinopathies can be grouped into 3 fundamental categories, the most relevant being the first 2:
– Structural variants of Hb, such as HbS (sickle cell anemia or sickle cell disease).
– Failure in the synthesis of an adequate amount of normal Hb (thalassemias) by default in the production of 1 or more of the globin chains.
– Failure in the normal jump that occurs in the neonate to produce HbF to HbA (hereditary persistence of fetal Hb).
The investigation of patients with suspected hemoglobinopathy should include a complete history with family history, physical examination and laboratory analysis. These tests were already defined in 1975 by a panel of experts from the International Committee for Standardization in Hematology: red series count with indices; Hemoglobin; hematocrit; peripheral blood smear; reticulocytes; iron metabolism; solubility test; falciformation test; quantification of HbA2 and HbF, and EF of Hb at alkaline pH. If the Hb detected is unstable or with affinity for the altered oxygen, the thermal stability (by heat) and chemical (isopropanol) test must be added. In this way, a reliable diagnosis can be made in most cases, although sometimes it is necessary to resort to more sophisticated techniques such as EF at acidic pH, the study of globins, isoelectric focusing or even molecular DNA analysis.
Electrophoresis in cellulose acetate at alkaline pH
This type of EF is routinely performed at pH 8.4-8.6 using a cellulose acetate membrane as a substrate, and is a simple, fast and sensitive method. Detects the most common Hb variants, and traditionally is the most used technique for the initial evaluation. At alkaline pH, Hb is a negatively charged protein that migrates to the anode (+) in an electric field. The Hb variants with different charges on their surface are separated from HbA and, therefore, all detected are different from it. Hb may be abnormal without change in the load, and therefore they will not be differentiated. With this technique, a separation of HbC, S, F, A and J is obtained. When a variant is detected, it is useful to quantify the percentage.
What difficulties of interpretation can be presented in this analysis?
– It can be difficult to detect minor bands such as Hb Constant Spring, HbA2, Hb Bart and HbH.
– In the neonate, in which there are small amounts of HbA and huge amounts of HbF, it can be difficult to detect HbA. That’s why you always have to resort to EF in citrate agar when HbA is not detected, or to use isoelectric focusing.
– It is not possible to differentiate between HbS, D and G. It is not possible to differentiate between HbC, E and O. Therefore, all samples in which a single band is detected in the HbS or C position should also be analyzed in citrate agar or with isoelectric focusing to exclude the presence of compound heterozygotes such as HbSD, SG, CE or CO.
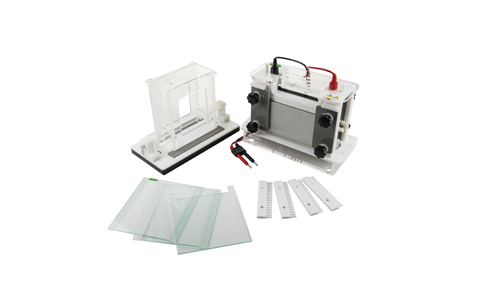
At Kalstein we offer you a high quality system with which you can perform hemoglobin electrophoresis, with very accurate results and great reliability. That’s why we invite you to take a look HERE