Diabetes insipidus is a rare but treatable condition that usually presents with polydipsia and polyuria. But distinguishing these symptoms from symptoms of primary polydipsia, diabetes mellitus and other causes of pollakiuria without polyuria can be very difficult. Diabetes insipidus is rare with a prevalence of 1 in 25,000 persons.
Central diabetes insipidus is usually caused by pituitary pathologies, either as a result of infiltrative or inflammatory processes or following surgery for a pituitary tumor, but may also be due to a congenital defect in the production of arginine vasopressin (antidiuretic hormone).
Nephrogenic diabetes insipidus is usually caused by electrolyte disturbances, nephropathy or pharmacological nephrotoxicity (commonly lithium).
Arginine vasopressin causes reabsorption of water in the collecting tubes of the kidney. Deficiency of the hormone or resistance to it, as in diabetes insipidus, leads to excess water loss by the kidney (polyuria).
Typically, the compensatory drive is thirst, which will provide adequate rehydration, but in severe cases, when there is no access to water, the person with diabetes insipidus can rapidly become dehydrated, which can lead to hyperosmolality, hypernatremia, and potentially death.
Symptom presentation
Extreme thirst and passing large amounts of clear urine are typical symptoms of diabetes insipidus, but it can be difficult to make a differential diagnosis with these symptoms, although indicators can be found in the history and studies, which may help.
In central diabetes insipidus, the history of polyuria and polydipsia is usually of sudden onset, presenting within weeks or months of onset. In nephrogenic diabetes insipidus, the onset is more insidious and patients usually have had symptoms for months or years prior to diagnosis.
Symptoms suggestive of pituitary disease are fatigue, dizziness, irregular menstrual cycles and galactorrhea in women, and loss of libido and reduced secondary sexual characteristics in men.
Disease research
The presence of diabetes mellitus should be ruled out, confirmed by formal measurement of fasting or random blood glucose. Serum electrolytes, diuresis and paired urine and plasma osmolality should also be evaluated.
Patients with suspected diabetes insipidus should be referred to a specialist for further investigations and treatment. The urgency of the referral depends on the severity of the symptoms.
If there is extreme thirst and polyuria and serum osmolality is >295 mOsmol/kg, shunting should be done within a few days or a few weeks at most.
Patients with known diabetes insipidus who have hypernatremia should be considered in emergency status, which should be resolved the same day.
Treatment
The therapeutic mainstays of central diabetes insipidus are adequate fluid replacement, treatment of the underlying pathology and administration of desmopressin. This antidiuretic hormone analog can be administered orally or by intranasal spray.
In general, central diabetes insipidus responds immediately to desmopressin, and patients notice a significant reduction in polyuria and thirst. Symptoms of insufficient desmopressin supply are thirst and polyuria, while symptoms of excessive replacement are headache and mild confusion (due to hyponatremia), and decreased urine output.
Nephrogenic diabetes insipidus is treated with fluid intake and specific etiological treatment under the care of a nephrologist. Other treatments include low sodium and high protein diets, diuretics and non-steroidal anti-inflammatory drugs.
It has recently developed recommendations for the inpatient management of acutely ill patients with diabetes insipidus. These guidelines recommend that all hospitalized patients with central diabetes insipidus be identified on admission and the appropriate endocrinology or clinical team be notified.
Any patient with central diabetes insipidus who is admitted to a hospital needs careful monitoring of fluid replacement, as well as appropriate administration of desmopressin.
It is recommended that hospitals develop an alert system to identify all patients requiring desmopressin treatment to ensure that medication is not missed.
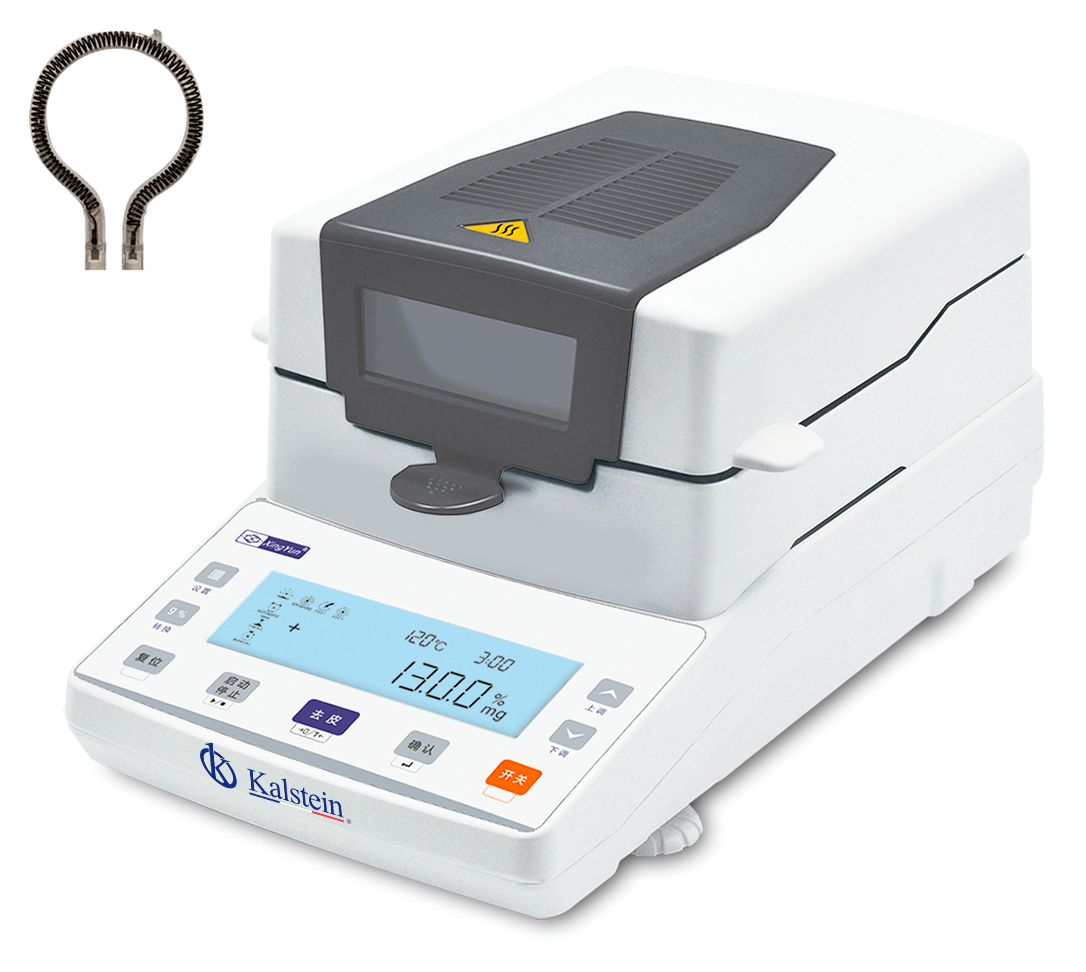
At Kalstein we offer you the digital brain electrical activity monitor, which generates a color electroencephalogram. It can be used to monitor diseases such as epilepsy, intracranial inflammation, cerebrovascular diseases and brain tumors, pituitary damage. Therefore, we invite you to take a look at: HERE